Worrying levels of sexually transmitted infections (STIs), including a steady rise in new cases and a high number of repeat infections, are fuelling concern among health authorities in Bulawayo, Zimbabwe’s second-largest city, amid fears that the trend could reverse gains made in HIV prevention.
Bulawayo National AIDS Council (NAC) Programmes Officer, Douglas Moyo said the city was witnessing patterns that pointed to persistent risky sexual behaviour, weak behaviour change, and heightened vulnerability to HIV infection.
Moyo said STIs remained a critical public health issue because of their direct link to HIV transmission.
“The topical issue now of sexually transmitted infections STIs. HIV is transmitted easily when one has a sexually transmitted infection. Why? Because sexually transmitted infections would provide easy passage through the breaking of the skin. Such that there is an easy entry,” he said to the media recently while giving the latest Bulawayo HIV Programmes Update.
Moyo explained that infections such as syphilis, gonorrhoea and chlamydia significantly increase susceptibility to HIV and act as markers of high-risk sexual behaviour.
“If you walk into any health facility, be it a private doctor or a clinic with an STI. This is clear evidence that ‘here is somebody who exposed themselves through having condomless sex or who had an accident somehow during the sexual encounter,’” Moyo said.
Drawing parallels with pregnancy, Moyo said STIs and PMTCT data both point to unprotected sex.
“Just like somebody who walks into a facility, they are pregnant, it’s evidence that they had unprotected sex, isn’t it? Because there is no way they could get pregnant if they were protected. So those two, PMDCT and STI, are key evidence of unprotected sexual intercourse. But the one that we are most worried about is this one -Sexually transmitted infections,” he said.
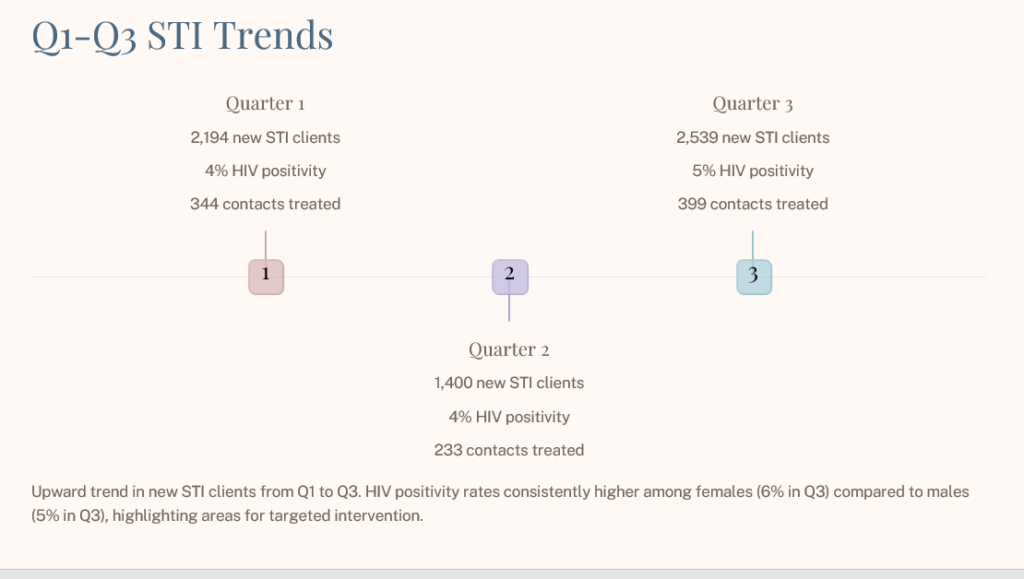
Data from the first three quarters of the year shows a troubling upward trend. In the first quarter alone, Bulawayo recorded 2 194 new STI cases.
“Look at the trend. Look at what happened in the first quarter. Quarter one, we had 2 194 new cases underline the word new and a quarter has only three months. In just three months, we recorded 2 194 STI cases,” Moyo said.
He said all STI patients are routinely tested for HIV, with the data revealing persistent HIV positivity among those presenting with STIs.
“And then the management protocol now for STIs is that anyone who presents with an STI should be tested for HIV. then we can see the positivity rate was 4 percent,” he said.
Although the number of new STI cases declined in the second quarter to about 1 400, Moyo cautioned against celebrating the drop without deeper analysis.
“Quarter two, the number declined. But that decline needs to be investigated, to say, was it a genuine or real decline, or is there something that happened with the data capturing? Because a decline from that to that, yeah, we need to find out,” he said.
“We need to find reasons if there were programmes, awareness sessions, or activities that resulted in that decline. We need to find out and celebrate those approaches because they did wonders but look at the positivity rate, again, it remained at four percent HIV positivity in the second quarter and we are talking about new cases.”
By the third quarter, new STI cases had surged again to 2 539, reinforcing concerns that Bulawayo was not making sustained progress.
“Then look at the last quarter, which is now, the previous quarter, the quarter three. We had 2 539 new STI cases,” Moyo said.
Moyo said when the first and third quarters are compared, the overall direction is clearly upward.
“When you look at the trend, if we are making any progress, look at the number in quarter one and compare it with quarter three, it’s going up. Don’t worry about the decline in the second quarter. If you were to draw a trend line of a graph, it would be going up,” he said.
“So if you were to draw a trend line from there, it would go down and then shoot up like that. That is a cause for concern,” Moyo added.
He stressed that STI cases also signal active sexual networks, increasing the risk of wider HIV transmission.
“Remember, for anyone who presents with a sexually transmitted infection, it’s clear evidence that they’re in a sexual network. How wide that sexual network is, no one knows,” he said.
“So it is a cause for concern if we continue to get 2 539 new cases by the end of last quarter,” Moyo said.
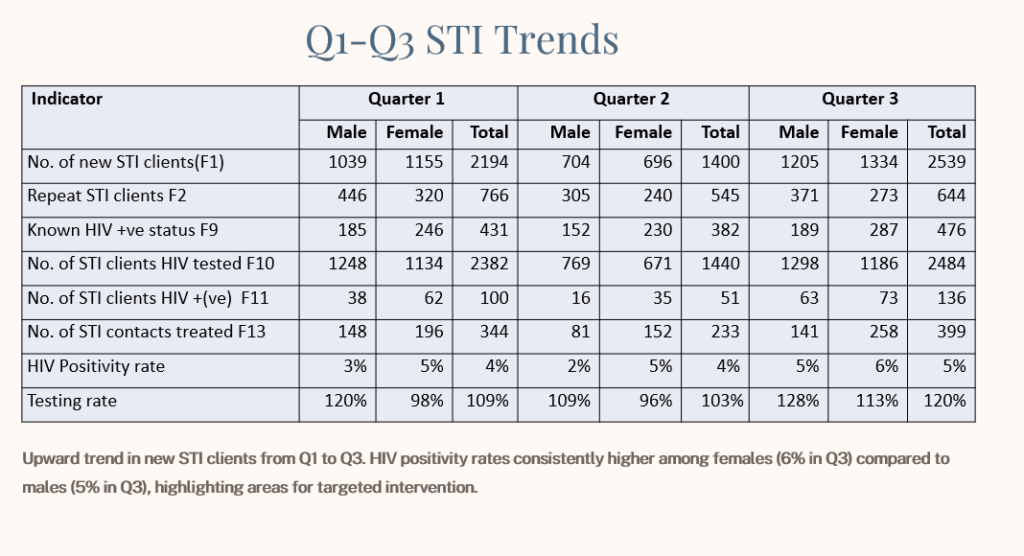
Moyo said the persistently high HIV positivity rates among STI patients show that HIV remains a serious threat.
“Somebody asked a question in one of the groups that is HIV still a threat? I think this is evidence to show that HIV is still a threat. If you can have a positive rate of four percent and it goes up to five percent,” he said.
He said fourth-quarter data was still being compiled and analysed.
“We are yet to analyse data for the fourth quarter because the year has not ended. December, I think, we are finishing our data collection next week. This is when we will analyse and see what this data is going to show us in the fourth quarter,” Moyo said.
Beyond new infections, Moyo said repeat STI cases were one of the most troubling indicators, showing limited behaviour change.
“Look at the repeat STIs, which is a cause for concern. When we talk about the repeat, we are talking about those people who are presenting to a facility, not for the first time at the STI,” he said.
Among males, repeat infections remained high across all three quarters.
“For males, I mean in the first quarter we had 766 repeat cases. In the second quarter we had 545. And then in the third quarter, 644 repeat STIs, which show that people are not changing their behaviour,” Moyo said.
He said repeat infections often result from failure to treat sexual partners and poor communication within relationships.
“A change of behaviour could mean that you have an STI. You have challenges or fears of approaching your significant other. You go and seek treatment clandestinely or privately, you get treated. But then you come back and get re-infected from the same partner because you didn’t discuss these issues,” he said.
Moyo emphasised the importance of partner notification and contact tracing.
“So when it comes to STIs, it is very important for sexual partners to be treated. Hence that programme of tracing the contact,” he said.
He said tracing sexual networks is critical to breaking cycles of reinfection.
“Then the sexual partner will be followed up. Then that other partner will be asked ‘who is your other sexual partner.’ So the whole network should be followed up and be brought to treatment,” Moyo said.
The high number of repeat cases, he said, points to persistent risk-taking and low self-perceived vulnerability.
“So the repeat cases, the repeats are a challenge. They are showing us that some people are not changing their behaviour. Some people still don’t perceive themselves as at risk of infection,” he said.
Moyo warned that this behaviour significantly increases the risk of HIV transmission.
“So if they can get repeat STI cases, what about the exposure or the risk of contracting HIV? It is heightened isn’t it?” he said.

