Bulawayo’s 2025 HIV Estimates Report has flagged persistently high infection rates among key populations, raising concerns over funding and programming gaps that threaten progress in fighting the epidemic.
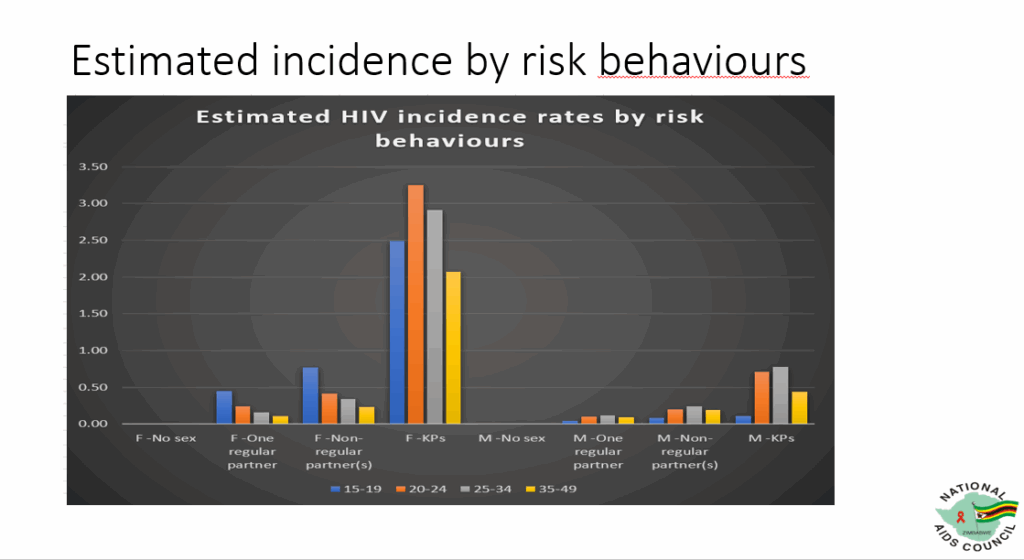
The data shows female sex workers and transgender women aged 20 to 24 bear the highest incidence rates, followed by men who have sex with men (MSM) and male sex workers in the 25 to 34 age group.
“Looking at incidence by risk behaviours, you find that rates are high among female key populations. When we are talking of female key populations, we are looking at our trans (transwomen) and sex workers. This is particularly evident in the 20 to 24 age group. Similarly, incidence is also high among male key populations, especially men who sex with men and male sex workers aged 25 to 34,” explained National AIDS Council (NAC) Bulawayo Monitoring and Evaluation Officer, Primrose Dube, during a recent workshop with journalists.
The findings expose both the health risks and invisibility of these communities, whose ‘hidden lives’ turn into ‘hidden risks,’ leaving some shocked at the very existence of men who have sex with men and male sex workers in Bulawayo.
Dube stressed that Bulawayo does indeed have male sex workers, something many continue to deny or dismiss.
“We have partners that are programming for key populations. We have the Sexual Rights Centre who are programming for men who have sex with men and are also programming for male sex workers,” she said.
“We also have the Centre for Sexual Health and HIV/AIDS Research (CESSHar) programming for female sex workers as well as male sex workers and trans (people). We have Trans Research Education Advocacy and Training (TREAT) programming for trans people and they are working again with all key populations, so we do actually have male sex workers in Bulawayo.”
Read https://cite.org.zw/bulawayos-silent-crisis-patients-defaulting-on-hiv-and-tb-treatment/ where in Bulawayo’s “silent crisis,” stigma-related stress drives many patients on HIV and TB treatment to drop out of care. Fear of judgment and discrimination leads some to hide their status, miss appointments and default on therapy.
Key populations such as female sex workers, transgender women, men who have sex with men, and male sex workers, face even harsher stigma at health centres, discouraging testing and consistent prevention. Excluded from most mainstream HIV programmes, they remain more vulnerable to infection and limited access to care.
In an interview with CITE, SRC Executive Director, Mojalifa Mokoele Ndlovu said from a programming perspective the organisation is more concerned about the level of risk associated with these groups rather than quantifying how significant the population is in Bulawayo.
“Men who have sex with men are disproportionately affected, probably 20 to 22 times more likely to contract HIV in their lifetime than heterosexual men. Sex workers are even more at risk, about 35 times more likely than women who have one partner. Transgender individuals also face high risks due to violence and discrimination,” he said.
“It’s those issues for us that make us worry when it comes to HIV prevention, that make us want to programme more, that make us want to engage NAC almost all the time to say, remember these populations and the risks that are associated with them.”
Ndlovu said it was crucial to integrate key populations into mainstream health services, avoid discrimination and reduce incidence risk.
“We really need to change the mindset of our service providers in public sector facilities. Sensitise and train our health care workers in public sector clinics and public sector hospitals so that they can offer non-discriminatory services, be welcoming, be friendly and have less attitude. So that these populations can be free, feel welcome and not afraid to go to public sector facilities,” he said.
“There is nothing that is more sustainable than going to a clinic that is just near where you stay.”
The SRC executive director also explained the impact of funding gaps, noting private clinics that offered inclusive services, like new start centres, stopped after USAID’s funding ended due to the ‘stop work orders.’
“So we have nowhere else to go,” Ndlovu said, noting key populations rely almost entirely on public hospitals and clinics.
“We need to make sure that NAC and Ministry of Health work closely with organisations like ours, SRC and others, train and make sure that nurses offer services without looking at if the person is a sex worker, is a transgender or the person sleeps with other men, but just offer the service based on the need ‘that has brought me to the clinic.’”
Ndlovu also addressed misunderstandings about male sex workers, stating it was “ignorance” to deny their existence and to assume male sex workers only sell sex to men.
“There are also male sex workers, who sell sex to women. We have men who actually charge women for sexual activities while of course there are other men who sell sex to other men,” he said.
“So sex work is a big industry. It’s very difficult to even understand the complexity of it but it’s happening. We are saying it’s happening because we work with men who sell sex to other men who will tell you that ‘my clients are high profile men, my clients are other men who come in and offer me this much for a short time, for a night, and so on.’”
By their very nature, key populations do not typically seek services in conventional health facilities and remain on the periphery of mainstream health provision.
“These realities should not shock us,” concurred one doctor who asked not to be named.
“Men who have sex with men, male sex workers, trans people and female sex workers exist in Bulawayo and across Zimbabwe. The data simply confirms what communities have known all along. These groups live hidden lives, which result in hidden risks.”
NAC’s M and E officer added that HIV estimates rely on surveys such as Zimbabwe Population-based HIV Impact Assessment (ZIMPHIA) and programme data from clinics, including HIV testing services, antenatal care and Voluntary Medical Male Circumcision.
These are fed into models such as NAOMI and Spectrum to produce projections.
“The current Ministry of Health and Child Care registers capture disaggregation by population type. Health care workers under BCC were trained on key population friendliness by NAC and its partners,” Dube said.
Bulawayo Provincial Medical Director (PMD), Dr Maphios Siamuchembu, also underscored the need for specialised programming as key populations require tailored interventions provided in safe spaces, which are resource intensive.
“That’s why they rely heavily on organisations that work directly with them,” he said, noting that these organisations also work with NAC.
“NAC is a parastatal of the Ministry of Health and Child Care, mandated with coordinating the response to HIV and AIDS. Their work is therefore Ministry work, and the data they collect belongs to the Ministry of Health and Child Care. NAC works with and coordinates all the partners in the HIV space and they collect data from all these partners. All this data filters to the Ministry.”
Dr Siamuchembu explained how challenges of providing services to key populations have been worsened by funding shortages, particularly after the United States government’s “stop work” orders that halted USAID-supported programmes.
“Especially after the US Government ‘stop work’ orders and closure of USAID programmes, funding gaps for key population interventions have increased. By their very nature, key populations do not seek health services in ordinary facilities. They require specialised programming, which is costly. This gap has worsened since the stop work orders,” he noted.
The PMD also pointed to severe understaffing within his department as some of the challenges.
“My office works with all organisations in health. The work of the Ministry of Health is very broad, but my office only has 10 authorised posts. This means we are severely short-staffed and cannot deliver everything expected of a Provincial Medical Directorate. I have therefore asked workers from sister organisations to double up and act in certain posts, even though some are not yet authorised,” he said.
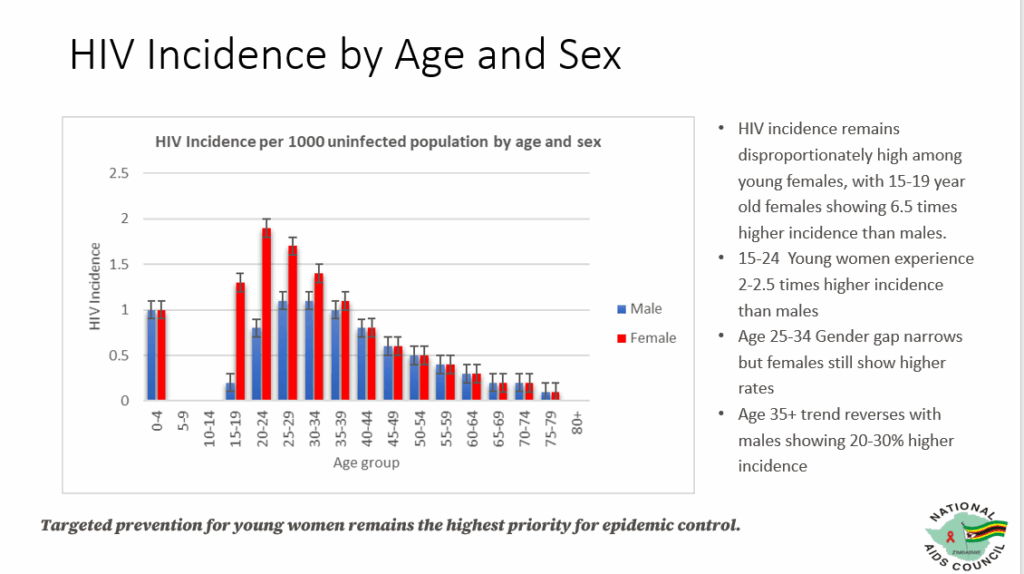
Meanwhile, the 2025 HIV Estimates Report report also shows that HIV incidence in Bulawayo remains higher among females aged 15 to 39.
However, from age 40 onwards, the trend reverses, with males recording higher rates than females.
“Looking at our HIV incidence by age and sex, from our last presentation that we had, we also had the same picture where the HIV incidence was actually higher among females from the ages of 15 to 19 to females of ages 35 to 39. So this picture is still the same for Bulawayo province, where females have a higher incidence from the ages of 15 up to the ages of 39,” said the NAC M and E officer.
“Then it flips and males have a higher incidence when compared to females from the ages of 40 going up.”
Dube highlighted that young women aged 15 to 24 remain particularly vulnerable, facing between two and 2.5 times higher HIV incidence rates compared to their male peers.
“For the 15 to 19 age group, in 2023 it was projected that females had a seven times higher chance of getting infected. In 2024, there was a slight reduction of 0.5 percent, meaning that the estimated incidence for girls in this age group was still 6.5 times higher than for boys. When we look at young women aged 15 to 24 overall, they continue to face between two and 2.5 times higher incidence rates compared to young men,” she said.
Dube added this underscores the urgent need for continued targeted prevention programmes.
“This basically means that as a province, we must prioritise prevention efforts for young women if we are to move toward epidemic control,” she said.
Support CITE’s fearless, independent journalism. Your donation helps us amplify community voices, fight misinformation, and hold power to account. Help keep the truth alive. Donate today


Leave a comment